Valium, Xanax, Ativan and Klonopin: Concerns for the Overuse of Benzodiazepine Medications
Stress and anxiety seem to permeate modern life. The World Health Organization estimates that 264 million people worldwide struggle with anxiety disorders (WHO 2017). And unfortunately, the incidence of anxiety disorders appears to be increasing.
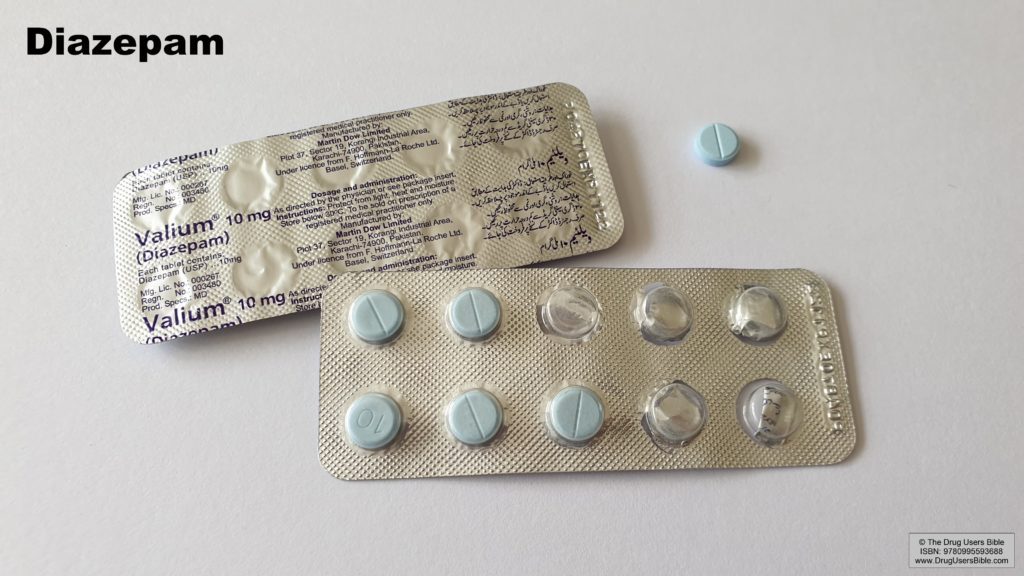
Standard first-line treatment approaches are counseling, including cognitive behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs) like Prozac, Paxil and Zoloft (Bandelow 2017). However, doctors often turn to benzodiazepines, a class of medications that includes Xanax, Valium and Ativan to treat anxiety disorders.
The Benzodiazepines
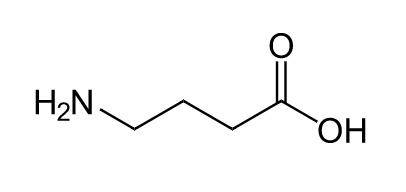
Benzodiazepines are a class of medication that act on the gamma-aminobutyric acid (GABA) system. GABA is the main inhibitory neurotransmitter throughout the brain. Benzodiazepines increase GABAA signaling which slows down brain functioning (Kim 2021). These effects are generally sedative and initially earned benzodiazepines the name of “minor tranquilizers.”
Since the sedative effects of benzodiazepines were safer than previous sedatives, they quickly increased in popularity. By the mid-1970s, Valium was the most prescribed drug worldwide (Kang 2020). Yet for years, the majority of the risks and side effects from these medications was downplayed and ignored.
Benzodiazepine Side Effects
Addiction
Benzodiazepines can lead to addiction and dependence. At standard therapeutic doses these drugs can produce “tolerance” where higher doses are needed to keep achieving the same effects (Soyka 2017). In practice, I often dread seeing patients on high doses of benzodiazepines due to the side effects and difficulty in stopping these medications. In patients with a history of alcoholism, benzodiazepines may also have a higher risk for addiction and abuse (Lejoyeux 1998).
Cognitive Decline
And while some of the data is conflicting, on the whole, benzodiazepine use appears to increase risks for cognitive decline, a precursor to dementia (Picton 2018). This is of particular concern in older patients. A recent review concluded that two-thirds of prescriptions in elderly patients for benzodiazepines were inappropriate. Older patients are at greater risks of side effects from these medications, including falls (with potentially lethal outcomes), accidents, dependence, worsening dementia and delirium (Airagnes 2016).
Death
Research findings on benzodiazepine use and increased mortality also raise concerns. In one large study, higher use of benzodiazepines increased risk of death by over five times. They were also associated with a 35% increased risk of cancer (Kripke 2012). While the findings are debated and risks seem to vary among specific benzodiazepines (Igbal 2015), there is a need for more research to fully understand and assess risks.
Opiates and Benzodiazepines
More recently it has been increasingly clear that benzodiazepines and opiates do not mix well. With the opiate epidemic, thousands of people have died from overdoses from both prescription and recreational use of opiates. When opiates are combined with benzodiazepines the risk of death is significantly increased (Boon 2020). Due to increased risks, it’s no longer recommended to prescribe the two medications together.
But…Do They Work?
One of the biggest questions around benzodiazepine medications is whether they are even effective at treating anxiety symptoms. While they have immediate and obvious sedative effects, the brain changes receptor levels in response, raising the need for higher doses. Recommendations for benzodiazepines have repeatedly stated the drugs should only be used short-term, generally up to four weeks (Ashton 2005). A review of the evidence from 2008 came to the stark conclusion that there was no solid evidence that benzodiazepines were even effective short-term for anxiety symptoms (Ladder 2008).
Even with recommendations against it, long-term use of benzodiazepines is common. And available data suggests that long-term use may make anxiety conditions worse (Guina 2018). A review on post-traumatic stress disorder and phobias clearly shows harms from benzodiazepines as treatment (Guina 2015, Cohen 1995). Studies suggest that benzodiazepines block “fear extinction,” meaning that fear responses persist and worsen anxiety long-term (Minnen 2002).
Patients struggling with anxiety often struggle with depression. Data potentially links benzodiazepine use with treatment-resistant depression (Parker 2015). Of equal concern, when patients successfully taper and eliminate long-term use of benzodiazepines, mental health parameters typically improve, highlighting the negative consequences of their use (Belleville 2008).
Discontinuation
If you have been on benzodiazepines long-term, it’s incredibly dangerous to stop cold turkey. Seizures and death can result. The best approach for discontinuing benzodiazepines is a slow taper assisted by a knowledgeable physician fully versed in the medications’ withdrawal symptoms and side effects.
Conclusion
Benzodiazepines like Xanax, Valium, Klonopin and Ativan are commonly prescribed for anxiety and insomnia. Yet, concerning data suggests these medications carry significant risks for harm with little data supporting efficacy, especially long-term. It’s likely these medications are vastly overused and patients would be better served with safer, more effective treatment options.



