Infection As a Cause of Depression

Depression is extremely common. Recent estimates suggest that 4.4% of individuals worldwide struggle with clinical depression (Friedrich 2017). In the United States, it’s estimated that one in five individuals will experience a major depressive disorder at some point during their lifetime (Hasin 2018).
Understanding the causes of depression is likely key for helping to address and reduce these numbers. Unfortunately, treatment is almost completely focused on just mental-emotional aspects and neurotransmitters to the exclusion of other factors.
Causes of Depression
Depression is a complicated illness that has physical, emotional, mental and spiritual dimensions. Often, depression is blamed on the individual for having a weak sense of self or poor coping mechanisms. If the depressed person could just think happier thoughts, everything would be fine. This often leads to blame and shame around depressive illnesses.
On the flip side, blaming depression solely on biochemical imbalances—often low levels of the neurotransmitter serotonin—can make individuals pessimistic about recovery (Deacon 2009). Patients may also doubt the benefits from non-drug based therapies that aren’t directly interacting with neurotransmitter levels.
The truth, as is often the case, is somewhere between the two extremes with numerous additional factors playing a role. An individual’s history, coping strategies and present stressors clearly affects mood. Nutritional factors, such as diet, also play a part. Individual nutrients that help prevent depression or reduce symptoms can also be key. Hormones clearly have an impact on mental health in both sexes, including sex hormones and thyroid function. Genetics can play a role as well. Inflammation can also be a major player affecting depressive symptoms.
Depression and Inflammation
Anything that increases inflammation in the brain, increases risks for depression. Evidence suggests that toxins, like heavy metals, plasticizers and pesticides all may increase risks (Koh 2017, Shiue 2015). Other causes of inflammation, like autoimmune disease, correlates with increased depressive symptoms (Pryce 2017). Acute and chronic infections can increase inflammation and appear to increase risks for depression and depressive symptoms as well.
Chronic Infections and Depression
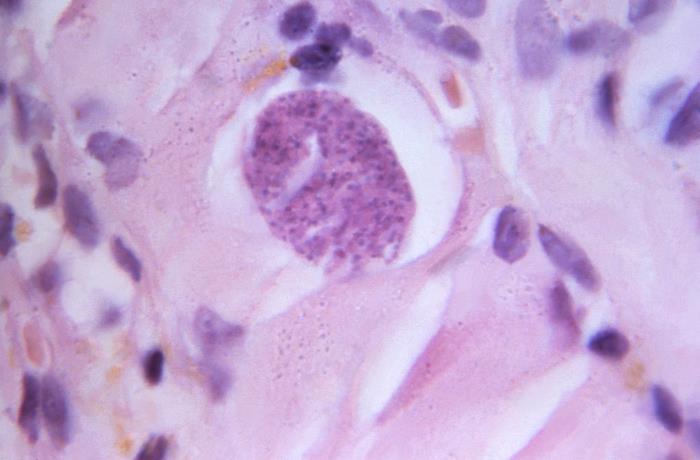
Evidence has been slowly accruing that chronic infections increase the risks for depression and other mental health problems. One of the more well-studied associations is between Toxoplasmosis gondii (T. gondii) infection and mental illness. T. gondii is commonly found in cats and transmitted by exposure to cat feces. Other animals can carry T. gondii and eating undercooked meat can also cause infection. Most individuals have no initial symptoms from exposure. The parasite then preferentially burrows into muscle and brain tissue where it encysts and remains dormant.
However, once present in tissues, an inflammatory response results. Since the immune system is typically incapable of clearing the infection, the inflammation becomes chronic. Ongoing inflammation from the presence of the cysts can cause or contribute to symptoms of depression, schizophrenia, and suicide (Hsu 2014). Studies suggest that upwards of 10% of the population has been infected with T. gondii (Dubey 2008).
And T. gondii is not unique in its ability to impact mental health. Viral infections are well known to have potential mental health consequences, including Human Immunodeficiency Virus (HIV), Epstein-Barr virus, herpes simplex virus type 2 and cytomegalovirus (Miller 2005, Gale 2018, Arseniou 2014). Once exposed to these viruses, they are generally persistent, with the immune system holding them in check over a person’s lifetime. Unfortunately, their presence leads to an increase in chronic inflammation which is what likely worsens mental health outcomes.
Other research also implicates bacterial infections as a potential cause of mental illness. Streptococcus is a bacteria commonly associated with strep throat. More recently, associations in children and adolescents between infection with Streptococcus and obsessive-compulsive disorder, tic disorders, attention-deficit/hyperactivity disorder and major depression has been found (Leslie 2008). When the infection is treated, symptoms typically improve or resolve.
Treating the Infectious Component of Depression
In patients struggling with depression and other mental illnesses, a comprehensive evaluation of potential causes and contributing factors, including inflammation and infections should be considered. While some viral and parasitic illnesses can’t easily be eliminated from the body, addressing the excess inflammation from their presence may still help reduce symptoms. If the infection is bacterial, it may require direct antimicrobial treatment. Just being aware of all the contributing factors that impact mental health can empower individuals to better understand their condition and affect resolution.
Conclusion
Depression is a complex illness with numerous factors contributing to symptom severity. Developing a more comprehensive understanding of and addressing the underlying causes will likely help to bring the current epidemic of depression under better control. Considering the number of patients still struggling to find significant relief, it’s worth expanding our understanding and approach to treatment.



