Is Low Progesterone the Cause of PMS?

While low testosterone levels and the related health problems are well studied in men, it’s long been hypothesized that a similar problem with progesterone occurs in women. The common belief is that low progesterone levels cause or contribute to premenstrual syndrome (PMS). Yet even though there are numerous web pages devoted to the topic of low progesterone, the research is thin and contradicts a lot of the standard beliefs.
Progesterone and estrogen are the two main female hormones involved with the menstrual cycle. During a normal cycle, progesterone is produced primarily in the second half of the cycle or the luteal phase. As progesterone levels fall at the end of the cycle, menstruation begins. As a hormone, progesterone prepares the uterus for implantation and is vital for maintaining early pregnancy. Low levels of progesterone are linked to problems with conception and miscarriage (Arck 2008).
Low Progesterone and PMS
While low levels of progesterone have long been thought to be associated with menstrual cycle symptoms, the research suggests a more complex situation. Some studies in women with premenstrual syndrome (PMS) have not found differences in estrogen or progesterone levels in comparison to women without symptoms, although the issue is poorly studied (Bäckström 1983). A more recent trial in healthy women found no correlation with mood symptoms related to any hormone tested, including estrogen, progesterone or testosterone (Hengartner 2017).
If low progesterone were the main problem causing symptoms during the menstrual cycle, you would expect that supplemental progesterone would be a simple solution. Yet studies on using progesterone as a treatment for PMS or premenstrual dysphoric disorder (PMDD), a more severe type of PMS, have mostly shown poor results. An older meta-analysis found no benefits, while a study from 2009 said the evidence was inconclusive (Wyatt 2001, Ford 2009). The results do not endorse the low progesterone theory as the cause of PMS.
Blocking Progesterone Eliminates PMS
Probably some of the strongest evidence comes from studies using medications that block progesterone production or its activity. A meta-analysis on the use of drugs that block the production of both estrogen and progesterone with or without estrogen added back, found that the drug regimen was more than eight times as effective as placebo for reducing PMS symptoms (Wyatt 2004).
A similar approach for PMDD also found benefits. In women with PMDD, a drug that blocks progesterone was also found effective (Poromaa 2023). In the study, 50% of women had complete remission of symptoms with the medication after three months. Another 35% found at least partial relief.
PMS and Allopregnanolone
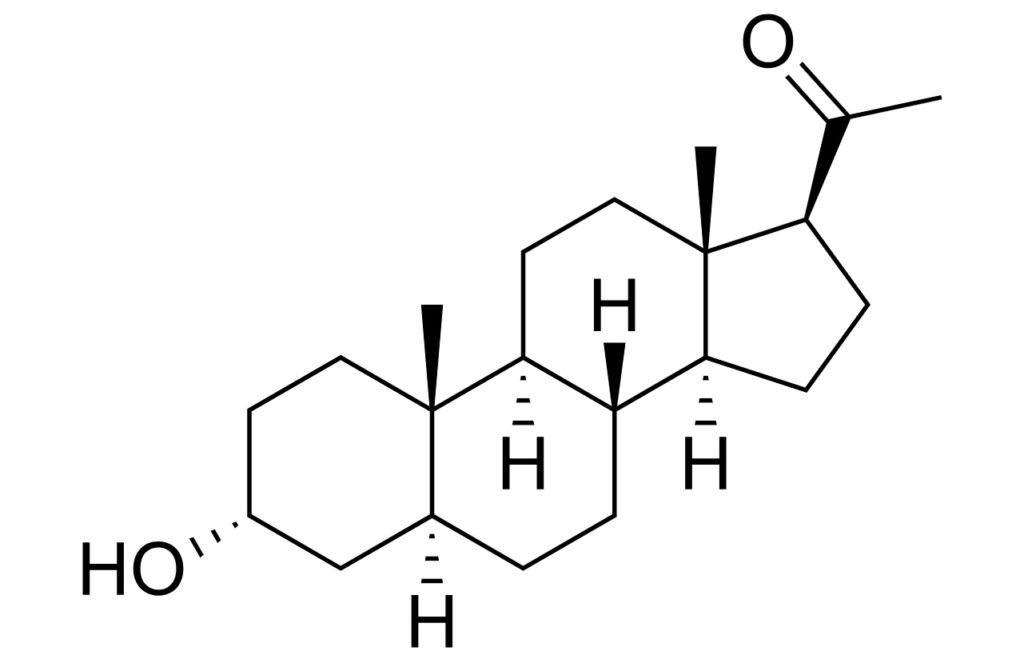
The majority of the evidence on hormones points to changing levels of progesterone causing problems for susceptible women. Typically, PMS symptoms follow elevated progesterone levels by five to seven days. If progesterone levels are held low and steady, symptoms typically do not occur. The findings suggest that a progesterone metabolite or downstream product called allopregnanolone may be the main culprit that contributes to PMS symptoms. Allopregnanolone is known to influence brain function. And studies in women with severe PMS, or premenstrual dysphoric disorder (PMDD), have shown altered brain responses to the hormone (Hantsoo 2020).
Therefore, blocking allopregnanolone may be a more direct way to stop PMS symptoms and still allow for a normal menstrual cycle. The approach appears to be effective for symptoms, although more research is needed. A small study that utilized a medication that blocks the production of allopregnanolone showed significant benefits for women with PMDD (Martinez 2016). Over a single cycle’s treatment six of eight women no longer qualified for a diagnosis of PMDD when allopregnanolone was inhibited. Further evidence confirming the relationship comes from a separate trial that utilized antidepressant medication to treat severe PMS. In the study, women that improved were found to have their allopregnanolone levels reduced as compared to those that had continuing symptoms (Freeman 2002).
Is Allopregnanolone Bad?
While allopregnanolone appears to cause PMS symptoms in certain women, assuming that allopregnanolone is bad is an oversimplification. Recent research shows very promising results using allopregnanolone injections for treating postpartum depression or baby blues. In 2019, a meta-analysis found that a single infusion of allopregnanolone for women struggling with postpartum depression was effective at rapidly providing relief that lasted for approximately one week (Zheng 2019). The situation highlights how in the right circumstances, allopregnanolone can be beneficial.
For women with PMS and PMDD, the problem appears to be a dysregulation of the normal response to allopregnanolone. Typically, the hormone is thought to interact with neurotransmitters that slow down brain activity. Slowing down brain activity is generally associated with improved mood and anxiety. However, for women with PMDD, allopregnanolone may slow down or decrease the function of the brain circuitry that controls emotions and the stress response (Bäckström 2011). By releasing the controls, emotions and stress become more acute and problematic. For these women with PMS or PMDD symptoms, stabilizing allopregnanolone levels may be an effective solution.
Conclusion
Some of the older simplistic beliefs that low progesterone is the main cause of symptoms around the menstrual cycle appear to be incorrect. In general, PMS symptoms are most likely related to the progesterone metabolite allopregnanolone that increases when progesterone levels increase in the second half of the menstrual cycle. Symptoms of PMS are often relieved by keeping levels of this metabolite stable. Hopefully, with more research, we can better understand the cause of the underlying problems with allopregnanolone to treat it more directly. While natural treatments can be effective for treating PMS and PMDD symptoms, as of yet, we do not know if or how they interact with allopregnanolone.



