Transcranial Magnetic Stimulation for Depression

Depression can be a challenging condition to treat, with standard medications often providing only minimal benefits. While there is a long history of electrical therapies being used for mental health conditions, they aren’t without controversy. Electroconvulsive therapy (ECT) is a treatment that runs electricity directly through a patient’s head causing a seizure. The treatment is thought to improve mood, but the data supporting its use is somewhat questionable at best (Read 2022). In addition, up to half of ECT patients have significant memory problems and damage that is often permanent (Read 2022).
In my own experience, I’ve seen patients with serious memory problems after ECT. One case in particular stands out: a younger patient who had ongoing depression and problems forming new memories after multiple ECT treatment sessions.
Transcranial Magnetic Stimulation
While historical treatments utilizing electrical equipment are controversial, one of the newest forms of treatment, repetitive transcranial magnetic stimulation, appears to show significant promise. The treatment differs from ECT as it doesn’t directly stimulate the brain with electricity, the treatment works through the production of an intense magnetic field.
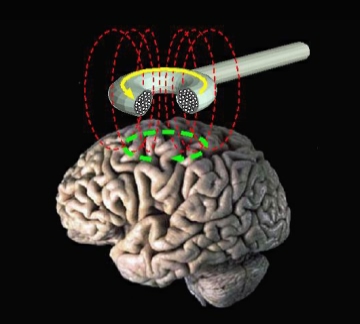
In some ways, transcranial magnetic stimulation can be thought of as a large, pulsed electromagnet. It works on the same principle as wrapping wire around a nail and hooking the wire up to a battery to create a temporary magnet. Transcranial magnetic stimulation uses a coil of wire that is placed close to a patient’s head. The coil is then briefly and repeatedly energized with large pulses of electricity. The magnetic field produced can penetrate into the brain and cause brain cells to fire. While not fully understood, these effects are thought to help positively influence brain circuitry, improving brain function and mood (Tik 2017).
Efficacy for Depression
In one of the first clinical trials, transcranial magnetic stimulation was able to reduce depression scores by 58% when combined with medication, as compared to just 28% with medication alone (Conca 1996). While promising, the study was small. Fortunately, additional clinical research was pursued.
The first meta-analysis of clinical trials of transcranial magnetic stimulation for depression found positive, but modest results. The authors noted that none of the included trials showed an average improvement of 50% or more in depressive symptoms. On average, 14% of patients halved their symptoms with treatment (Holtzheimer 2001). While modest, when compared to the average small effect size of standard medications, it’s worth noting the potential superiority of transcranial magnetic stimulation for treatment.
More recently, the data appears to have improved with additional research. A meta-analysis from 2019 found that one-quarter of patients treated with transcranial magnetic stimulation had their symptoms of depression decreased by half, while 16% of patients achieved full remission (Sehatzadeh 2019). It’s obviously not a cure for everyone, but a significant percentage of patients do experience benefits with transcranial magnetic stimulation.
Safety
Overall, the research strongly suggests that transcranial magnetic stimulation is safe, with minimal side effects. The main reported issues are transient headache, discomfort and pain at the treatment site. However, these side effects were not typically severe enough to cause patients to discontinue treatment (Wang 2022).
Unlike electroconvulsive therapy, which often causes memory damage, preliminary data suggests that transcranial magnetic stimulation is beneficial for brain function. Initial studies in dementia patients have shown improvements in cognition and memory (Lazzaro 2021)
Costs and Availability
Notably, one of the biggest challenges for patients to receive transcranial magnetic stimulation is the cost and insurance coverage. Generally, patients have to have failed to respond to multiple antidepressant medications before transcranial magnetic stimulation can be considered for insurance coverage. The total course of treatment costs between $6000 and $12,000. In addition, patients may need occasional retreatment to prevent the recurrence of depressive symptoms, which may not always be covered.
Conclusion
Transcranial magnetic stimulation is a newer treatment for depression that appears to hold significant promise for the relief of depressive symptoms in some patients. It also appears to be well tolerated with mild, transient side effects for most individuals. Hopefully, access to transcranial magnetic stimulation will increase, allowing more people to have a non-drug option for depression treatment.




Thanks for explaining how TMS works as a form of therapy that can reduce the symptoms of depression. I heard rumors that my colleague has been battling similar problems recently while at work. We should probably find a TMS professional that can help him try this therapy someday.
I know people who have responded well to TMS for depression. It is definitely worth considering as a treatment option.